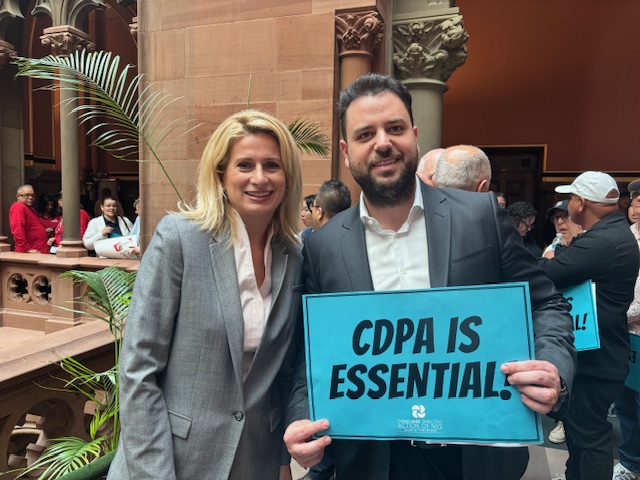
The Budget negotiations are winding down in New York State and even though we have not yet received any final and official Budget language, last night, the Governor summarized the key provisions of the State’s upcoming FY budget (see minute 57 of the speech HERE for the relevant statements). As relevant to our readers, the Budget will include law that will consolidate almost all of the fiscal intermediaries.